Most First Strokes Are Preventable - 10 Habits Proven to Work According to the New 2024 AHA/ASA Guideline
A lifestyle-only plan distilled from the 2024 AHA/ASA primary prevention guidance.
Welcome to the Healthy Aging Newsletter, a free publication translating trustworthy medical research into simple habits to age well, free of chronic disease. I’m Dr. Ashori, a family medicine doctor turned health coach.
1 in 4 adults will have a stroke. Most first strokes are preventable with day-to-day habits, without fancy tests. This guide turns the 2024 AHA/ASA primary prevention guideline into actions you can start this week in your 30s–40s.
TL;DR
Check your health markers & repeat regularly.
Eat a Mediterranean-style pattern, most days.
Move more & break up sitting.
Master home BP skills & aim lower.
Quit nicotine & remove secondhand smoke.
Sleep 7–9 hours; screen for sleep apnea.
Eat fiber-rich carbs & watch your waist.
Improve lipids via food choices, not pills.
Find female-specific risks early.
Skip most supplements.
Quick self-check
Blood pressure: aim <130/80 at home; measure the right way.
Waist-to-height: target <0.5.
Weekly movement: ≥150 min moderate or ≥75 min vigorous.
Tobacco/nicotine: none; remove secondhand exposure.
Sleep: 7–9 h; screen for sleep apnea if snoring.
Diet pattern: Mediterranean-style most days.
The reason we call it “primary prevention” and “first stroke” is because some people already had a stroke. I wrote this guide for those who have never had and hopefully never will have a stroke.
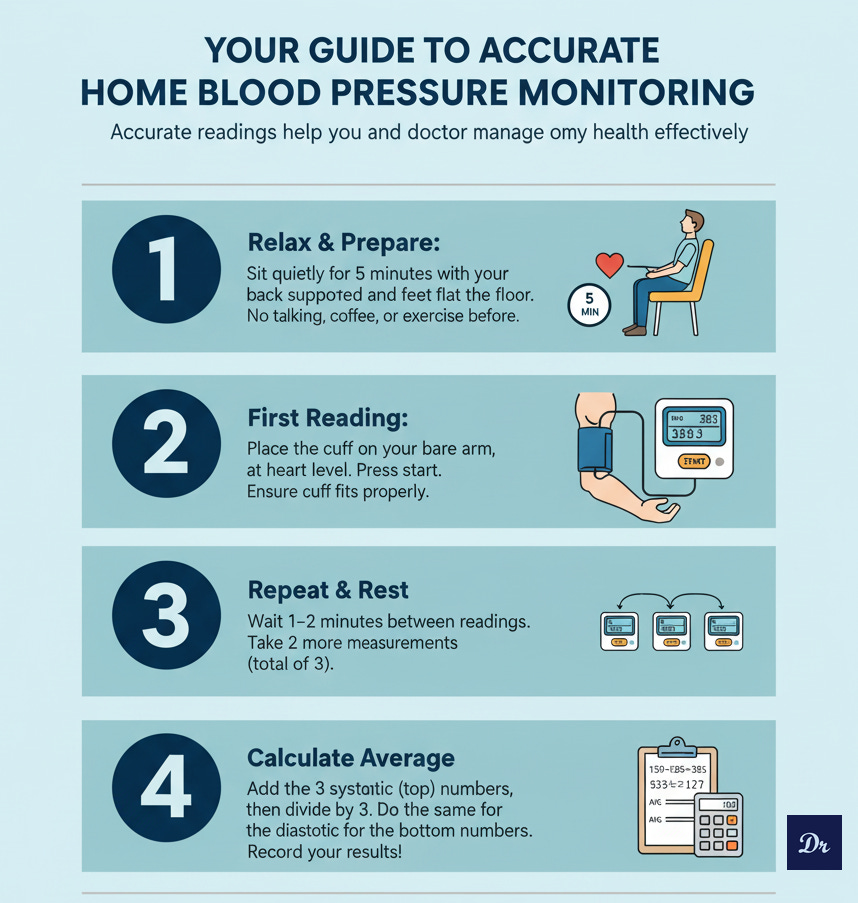
1) Master Home Blood Pressure Skills
Why it matters: Blood pressure control is the most powerful stroke-prevention lever. Small errors in measurement can be very misleading.
Action steps
Use a validated cuff; sit 5 minutes; arm at heart level.
Average readings: 2–3 readings, twice daily, for a week when adjusting.
Work the levers: Mediterranean eating, less sodium, exercise, weight, sleep.
2) Quit Tobacco and Nicotine
Why it matters: Nicotine and smoke exposure sharply raise stroke risk. E-cigs are not the best way to quit.
We have more tools than ever before to help someone quit cigarettes. And if you can’t quit, even 1 cigarette less per week will have a major impact on your overall health.
Action steps:
Combine meds + counseling for best quit rates.
Remove secondhand smoke from home and car.
Do not swap to e-cigs as your “treatment plan.”
3) Move More, Sit Less
Why it matters: Physical inactivity and prolonged sitting raise stroke risk; activity goals reduce it.
Action steps:
Weekly movement goals: 150 min moderate or 75 min vigorous activity weekly.
Strength 2 days/week.
Break up sitting every 30–60 minutes with 2–3 minutes light movement (set a timer)
4) Eat a Mediterranean-Style Pattern
Why it matters: Mediterranean-style eating lowers stroke risk and improves many other risk factors.
Action steps:
Focus your meals on vegetables, legumes, whole grains, fruit, nuts, olive oil; seafood 2×/wk; minimize refined grains (white rice, white flour) and processed meat.
If older than 60 with uncontrolled BP, consider salt-substitution (potassium-enriched) instead of table salt.
Use herbs/citrus to cut salt craving in home cooking.
Best salt strategy: Train your taste buds to crave salt a little less and use salt substitutes, herbs, and citrus to scratch the salt itch. Taste is a habit!
5) Fiber-Forward Carbs + Weight Awareness
Why it matters: Higher fiber and healthier weight improve blood pressure, lipids, and glucose, lowering stroke risk.
Action steps:
Build plates around legumes, intact whole grains, fruit, and veg.
Replace refined grains and sugary drinks.
Track waist-to-height and make tiny weekly changes that compound.
6) Sleep Well + Screen for Sleep Apnea (OSA)
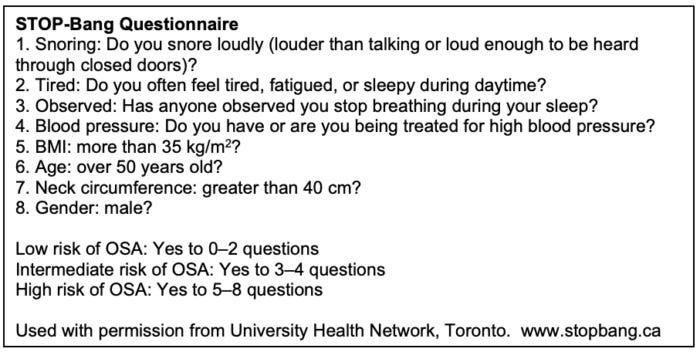
Why it matters: Sleep apnea (OSA) increases vascular risk; treating OSA may reduce stroke risk. It also helps with dementia prevention, better metabolism, and daytime fatigue. And it’s easy to screen for it without any gadgets or tech.
Action steps:
Screen if red flags: Loud snoring, witnessed apneas, resistant hypertension, constant sleepiness (use the STOP-BANG calculator)
When OSA is confirmed: Use CPAP as prescribed or weight loss.
Protect sleep: Consistent schedule, dark cool bedroom, limit alcohol late.
7) Know Your Baseline
Why it matters: The risks for a stroke are often silent. Catching them early changes your long-term curve. Things like inflammation, blood pressure, sleep apnea, and metabolic problems are often silent.
Action steps:
Annual tests: Blood pressure, heart rate, weight, waist circumference.
Every 1–5 years: Cardiovascular risk estimate through labs and tests (higher risk = more frequent screening)
Identify barriers: food access, sleep, stress; plan around them.
8) Improve Lipids With Food Pattern
Why it matters: Certain lipids in the blood drive ischemic stroke risk; diet quality lowers these ApoB, LDL-C, Lp(a), and TG particles.
Action steps:
Swap saturated fats for olive oil, nuts, and legumes.
Choose fish over processed meat.
Make dessert fruit-forward and minimally sweetened.
9) Female-Specific Risk Flags
Why it matters: Certain medical histories in females raise risk for early stroke. Specifically, it has to do with estrogen levels which can be affected by endometriosis, early menopause, or birth complications.
Action steps:
Tell your clinician about adverse pregnancy outcomes, endometriosis, early menopause, high BP during pregnancy, gestational diabetes, placental abruption, small-for-gestational-age infant.
Use lower-dose estrogen if choosing combined hormonal contraception.
Transgender women and gender-diverse individuals have the added estrogen risk.
Female-specific flags: adverse pregnancy outcomes, early menopause, endometriosis, and estrogen therapy. There are safe ways to manage these risks but your doctor should know about them and know what to do about them.
10) Skip Supplements With No Proven Benefit
Why it matters: Popular supplements have not decreased the risk of developing a stroke. Instead of supplements, consider spending the money and effort on habits & lifestyle changes.
Action steps:
Do not rely on multivitamins, antioxidant vitamins, calcium, or fish-oil capsules to prevent stroke - the data doesn’t prove it.
Invest in groceries, not supplements - the proof is very strong here.
Don’t waste money: supplements listed as no benefit for primary stroke prevention.
7-day Starter Plan
Daily anchors: 1 Mediterranean plate, 30+ minutes of movement, break up sitting, 7–9 h of sleep.
Day 1: Stock pantry with olive oil, lentils, canned chickpeas, oats, nuts, frozen veg, tinned fish. 30-min brisk walk. Check your BP (blood pressure).
Day 2: Lunch bowl with lentils + quinoa + roasted veg + olive-oil vinaigrette; stand/move 3 min per hour. Schedule a tobacco quit plan.
Day 3: 25-min jog or cycle + 10-min strength. Swap high-salt processed foods for home-cooked; improve taste with herbs and citrus.
Day 4: Fish + bean salad + whole-grain bread + olive oil. Evening wind-down: fixed sleep window; screen for sleep apnea if snoring.
Day 5: 5×3-min faster pace or light jog (fast walk + slow walk). Add a ‘no-sugar beverage’ rule today. Recheck BP.
Day 6: Make a meatless day with bean chili or chickpea stew; nuts for snack. Replace TV hour with a stroll.
Day 7: Meal prep 3 fiber-rich lunches; set weekly reminders for BP, steps, and grocery list. If overweight, set 0.5–1 lb/week loss target by restructuring dishes.
Mini-FAQ
Are salt substitutes OK? Usually. Potassium-enriched salts can help you get the same taste with less sodium and more potassium.
Should I use e-cigs to quit? There are far better methods to quit cigarettes; from hypnosis to nicotine to medication.
Do I need a sleep study? If you snore loudly, were told you stop breathing in your sleep, or have resistant hypertension, get screened. It’s easy and cheap.
How often to check BP? If you’re borderline, check weekly. If normal, only every few years.
Do fish-oil capsules prevent stroke? They don’t. Focus on your diet and other lifestyle habits.
If content like this is valuable please consider subscribing and sharing. If you want help lowering your risk of stroke, consider booking a one-on-one session with me, Dr. Ashori MD.








This is an excellent and actionable distillation of the new guidelines, Dr. Ashori.
What's powerful here is viewing these not as a checklist, but as a synergistic system for reducing the total inflammatory and endothelial load on the vascular system. Each habit, from improving sleep architecture to managing blood pressure, isn't just a separate lever. They are interconnected dials on a central control panel that governs vascular integrity.
You can't turn the 'diet' dial to 10 and ignore the 'sleep' dial set to 2 and expect the system to function optimally. It’s a masterclass in treating the body as the integrated system it is, rather than a collection of isolated risk factors.
Great work translating complex guidelines into a clear, actionable protocol.
Dr Tom Kane
Great advice Dr Ashori! Agree with your lifestyle first (exercise and nutrition) over supplements without proven benefit.