Fix Your Back Pain Fast - 8 Types of Back Pain & What to Do
A plain back guide from fascia to nerves, to keep you away from surgeons and medications.
My health coaching practice is all about prevention. And once something like back pain sets in, my secondary goal is to avoid unnecessary treatments, surgeries, or disability due to the pain. This is the best way to get back on track after experiencing back pain.
This guide reviews the common back pains and the right next steps to help you recover. You can experience back pain without suffering from it or having it negatively impact your life.
Too many patients end up in the revolving door of testing, treatment, surgery, retesting, pain meds, and more surgery. That’s what this guide is meant to prevent.
TL;DR
Back pain is prevented through mobility, stability, and strengthening.
Most back pain can improve in 6–12 weeks without surgery.
Start with activity, education, targeted exercises, and analgesia, as needed.
Match treatment to pattern. Escalate only if red flags or failure to improve.
Imaging is for red flags or persistent neurological deficits.
Track function, not just pain, to avoid dependence on pain meds.
This guide is to help you discuss your health more deeply with your clinician, not for self-diagnosis.
Identify Your Back Pain
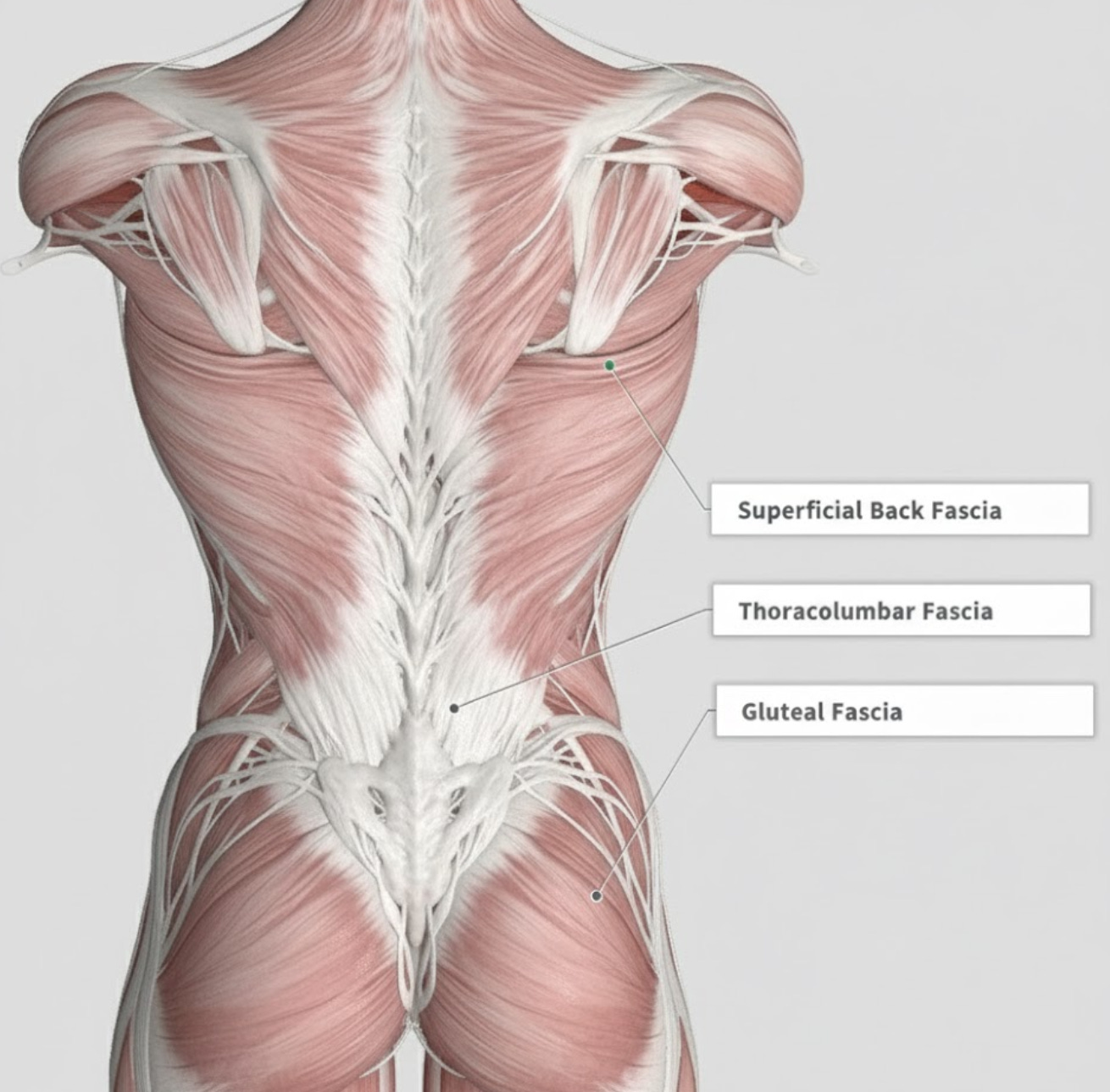
Most back pain comes from irritation of the fascia in the back and muscle spasms - not herniated discs. Achy and throbbing, often worse with sitting and better after some movement - that’s usually soft tissue irritation. Sometimes called, myofascial strain.
The most common underlying causes are deconditioning & overtraining.
Before visiting your doctor, take some time to better understand your back pain. These questions will help you have a much more fruitful conversation with your clinical team.
Know the answers to these:
Does the pain travel past the buttock, for example, down to the foot?
Do you have true weaknesses, such as foot drop?
What makes it better/worse, extension, flexion, loading, rest?
Is the area tender to touch or specific movements?
Is there an activity pattern that routinely sets off your pain?
1. Muscle Weakness (25-40% of cases)
The most common complaint is an ache with standing or walking, poor endurance, and we usually see a lot of swayback or anterior tilt of the pelvis. This is partially due to genetics but also from a lifelong posture routine.
Best treatment options:
Progressive core and glute muscle strengthening and hip hinge training.
Strengthening of the muscles in the hip and upper legs.
Endurance walking after movement is improved.
Improving mobility in the hip flexors and ankles.
Most muscle-weakness back pain shows up in people in their 40s and 50s. You can be fit or sedentary and still get it. The good news is it responds well to the right plan.
I have the same pattern. I had one bad night when I panicked and could not sleep. A friend gave me a simple plan. By the next day the pain eased and I’ve managed it really well since.
Now I get small flares, but they are brief. It has not stopped me from doing what I love. With steady strength work and smart movement, you can get there too.
2. Myofascial Tightness (15-30%)
Morning stiffness, relief with heat and gentle movement, and even more vigorous exercise is the hallmark of myofascial pain patterns in the lower back.
Best treatment options:
Heat, self-massage, foam rolling, mobility drills, yoga.
Work your way towards more movement gradually.
Accept worsened pain before improving.
3. Too Much Sitting (10-15%)
Sitting changes the architecture of the pelvis, hips, and lower back. Back pain develops after long sitting, relieves with standing, and involves tight hip flexors and hamstrings.
Best treatment options:
Take frequent microbreaks from sitting.
Mobilize your hip flexor and hamstrings.
Try standing work blocks and some longer walks.
4. Piriformis Syndrome (5%)
Piriformis syndrome is often felt as a deep ache in the buttock that worsens with sitting, with point tenderness over the piriformis and occasional tingling down the leg. Sitting cross-legged or slouching at a desk tightens the muscle and irritates the nearby sciatic nerve, so symptoms flare.
This is often misdiagnosed as “sciatica” which is a nerve root problem near the spine. Piriformis is the irritation of the sciatic nerve as it courses through the buttock muscles.
Best treatments:
Piriformis and hip external rotator stretching
Glute strengthening & gentle neural glides.
Adjust posture at the desk or sitting on the affected side.
Trigger point work may also help but only as an adjunct.
5. Sciatica From Nerve Root Irritation (5-10%)
Low back or buttock pain that shoots past the knee. Often with tingling or numbness. Sitting or bending over to tie your shoes can set it off. Even rolling over in bed can be painful.
Best treatments:
Do gentle backbends. If that hurts, try gentle knee-to-chest.
Walk a little more each day. Short, frequent walks.
Do gentle nerve moves: sit tall, slowly straighten one knee, then bend it again.
Start physical therapy early.
6. Suspected Disc Herniation (3-5%)
Disc herniation usually starts with sudden low back pain after a lift or twist. Pain can run into the leg. Bending forward makes it worse. The good news is that most disc herniations shrink back on their own.
Best treatments:
Gentle backbends if they reduce pain.
Keep moving with short walks; avoid bed rest.
Epsom salt baths can help.
7. Facet Joint Pain (5-10%)
Facet arthritis and SI joint pain are often worse with standing, twisting, stairs, or leaning back. Often easier with a slight forward bend.
Best treatment options:
Core bracing and simple trunk holds.
Hip mobility drills.
Spine decompression by hanging.
Walk daily.
Stay out of painful end-range backbends early.
8. Spinal Stenosis (1-5%)
Spinal stenosis isn’t common but with age the risk goes up. Legs feel heavy or tired when you walk. Pain eases when you sit or lean forward, like over a shopping cart and it’s a gradual process.
Best treatment options:
Do “forward-friendly” exercise. Cycling or walking while slightly bent forward.
Walk in short intervals. Rest, then repeat. Build time each week.
Add simple core and hip endurance work.
Manual Therapies That May Help
I’m a big fan of trying different modalities before dismissing them. If you believe it might help it’s worth trying.
Acupuncture: Can ease pain for a short time. Use as a helper, not the main plan.
Massage: Good for short-term relief and relaxation. Pair it with exercise.
Chiropractor: Fine for new or recent back pain without nerve signs. Avoid forceful moves if you have numbness, weakness, or other nerve problems.
Medications & Heat
Heat, topical NSAIDs, acetaminophen, and topical capsaicin cream.
Short oral NSAID course if needed, avoid long use.
Muscle relaxants only short term at night if spasm. Usually not too effective.
Imaging & Red Flags
Get seen right away if:
Cancer history, fever, or chills
Unplanned weight loss
High infection risk
Major trauma
Long-term steroid use
Osteoporosis with sudden pain
New or worsening numbness or weakness
pelvic numbness, trouble peeing or pooping
The thing about MRIs is that they often show “problems” that are normal with age. Disc bulges and arthritis are common in people without pain and once it’s seen on an MRI it’s hard to unsee it.
Chronic Back Pain & Pain Medications
The problem with taking long-term medication for pain is that, one, you develop a tolerance to it. Second, long-term use increases the risk of medication side effects. Third, you sensitize your body to be more pain-sensitive.
The solution isn’t to avoid pain medication but to retrain the brain to assess pain. If you’ve lived with back pain or any pain long enough, your brain and nerves have developed a heightened response to pain.
The good news is that you can reprogram this pain pathway through proper biofeedback, cognitive behavioral therapy, hypnosis, and other therapies.
Mini-FAQ
Do I need an MRI?
Usually not. But let your medical team know about your symptoms and definitely consider imaging if any red flags exist.
Is cracking my back harmful?
If it doesn’t cause you pain, it’s not a problem. If you have severe osteoporosis, be cautious.
Which mattress should I use?
The one that’s most comfortable. But the idea that your mattress will cause or fix your back pain doesn’t hold up in research.
Can I lift weights?
Always ease into it gradually. And, yes, it’s almost always a good idea.
When do injections help?
Epidural injections can be helpful but rarely are a cure. They are a good option when all other options have been tried.
The information in this podcast is for general education. It is not medical advice. Listening does not create a patient–doctor relationship with me. I care about each listener and want you to receive care that fits your life and medical needs. Always speak with your own licensed clinician before starting, stopping, or changing any health plan, medication, or routine.